Another Slow Year for Health Care Cost Growth
On Monday, the Centers for Medicare and Medicaid Services (CMS) released their annual update on health care spending growth, showing that 2012 was another year of slow cost growth and lending further insight into the burning question of what’s causing the recent slowdown.
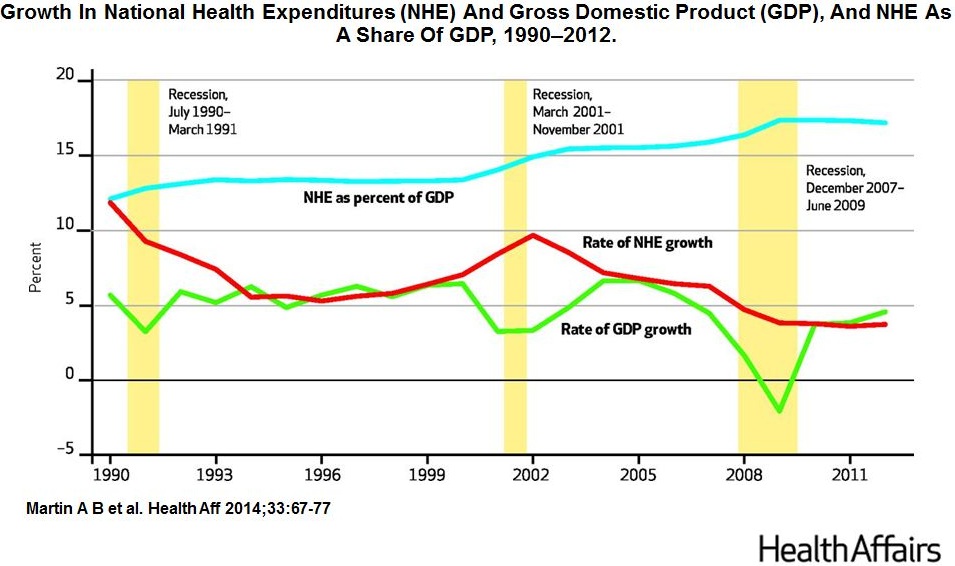
National health care spending grew by 3.7% in 2012 to $2.8 trillion, or 17.3 percent of the economy (GDP), continuing the recent trend of relatively stable slow growth since 2009. National health expenditures (NHE) actually declined as a share of GDP this year (from 17.1 percent in 2011). Moreover, this stability follows a steady slowdown in growth since 2003. The paper explains that “faster growth in hospital services and in physician and clinical services was mitigated by slower growth in prices for prescription drugs and nursing home services.”
Despite a growing debate over what is causing the slowdown, the CMS National Health Expenditure Accounts Team (who published the data) maintain that “the relative stability since 2009 primarily reflects the lagged impacts of the recent severe economic recession.” Further, they argue that “this pattern is consistent with historical experience when health spending as a share of GDP often stabilizes approximately two to three years after the end of a recession and then increases when the economy significantly improves.”
They make clear, however, that more evidence is needed to make any firm conclusions. In particular, the authors show that part of 2012’s slow growth was attributable to the increase in the use of high-deductible health plans and a number of high-volume, high-cost drugs going off patent in 2012 (most notably Lipitor, Plavix, and Singulair).
Although Medicare had the biggest increase in enrollment since its inception as the baby boomers started to reach retirement, Medicare spending per enrollee slowed to only 0.7 percent in 2012, down from an already low 2.5 percent growth in 2011. The authors explain that the added slowdown is largely result of a payment cut for nursing home services, enacted in the Affordable Care Act (ACA). Other provisions enacted in the ACA also contributed to this decline. Some were one-time cuts like lower reimbursements for Medicare Advantage plans, while others (like the annual productivity adjustments to payment updates for hospitals and other providers) should have a more a permanent effect. 2012 also saw slower growth in Medicare inpatient admissions, which might be in response to the ACA’s readmission penalties.
Key Takeaways
- Health care cost growth, across-the-board, continues to remain subdued.
- The Baby Boom generation is hitting retirement. “Enrollment in Medicare for all beneficiaries (fee-for-service and Medicare Advantage) jumped 4.1 percent in 2012—the largest one-year increase in enrollment in thirty-nine years.”
- Medicare Advantage plans are getting really popular. The private insurance plans offered as an alternative to traditional Medicare, primarily in the form of closed network health maintenance organizations (HMOs), were chosen by “more than half” of new Medicare enrollees in 2012.
- High-deductible plans continue to grow in popularity. “Net enrollment gains in high-deductible plans contributed to the slow growth in premiums. Enrollment in high-deductible health plans, which generally have lower premiums and higher cost sharing than other more popular plans, accounted for 19 percent of all covered workers and 31 percent of the under-sixty-five insured population in 2012.” The growing use of high-deductible plans and more limited networks among the under 65 population might help explain the increasing popularity of Medicare Advantage plans when those people turn 65.
- The “Patent Cliff” is lowering health care spending. Part of the explanation for the recent health care slowdown is generally attributed to a slowdown in prescription drug expenditures, and the authors show that a few blockbuster medications going off-patent in 2012 reinforced this trend. It is unclear, however, what the recent deceleration in the development of high-volume, life-changing drugs portends for future innovation.
If the current slower trend in national health expenditures continues, families, businesses, and governments will all greatly benefit. The most optimistic take comes from David Cutler and Nikhil Sahni of Harvard, who find that only 37 percent of the slowdown experienced from 2003 through 2012 was the result of the recession. The study argues that the decelerating development of new expensive technologies and the rise of high-deductible health plans played a significant role.
If the increase of high-deductible and managed care plans has helped depress health care spending growth, parts of the Affordable Care Act could bolster this trend. By relying on premium cost competition, the ACA marketplaces promote the use of these plans, and the pressure on employer-provided insurance premiums from the Cadillac Tax will likely have a similar impact on the employer market. The increasing popularity of managed care plans in Medicare may also be a sign of Americans’ growing comfort with limited networks and higher deductibles.
Both this study and various other analyses, however, should inspire caution against declaring victory prematurely. A study from the Altarum Institute and Kaiser Family Foundation suggests that 77 percent of the recent slowdown can be explained by the economic doldrums and another study from Chandra, Holmes, and Skinner of Harvard suggests that excess health care spending growth will eventually return to 1.2 percent faster than economic growth. These studies and the CMS National Health Expenditure Accounts Team note that the current slowdown is still consistent with historically lagged effects of recessions. The blowback to the rise of managed care in the late 1990s and resulting higher spending growth, in particular, should serve as a harrowing memory.
Moreover, many of the perverse incentives that have plagued the health system for years still remain in place. Only 11 percent of payments to doctors and hospitals are based on quality and value, according to Catalyst for Payment Reform. Most beneficiaries in Medicare are still insulated from cost-sharing by prevalent supplemental coverage that distorts incentives. This insulation also makes it more difficult for Accountable Care Organizations (ACOs) to succeed in Medicare since enrollees will have no financial incentive to see providers within the ACO rather than potentially more expensive alternative ones.
Only time will tell whether the slowdown will persist. In the meantime, lawmakers should work to figure out what factors are having salutary effects and reinforce them. The effort to replace the sustainable growth rate with structural reforms to the Medicare payment system is a good place to start.