Two New Ideas to Save Money on Drugs in Health Affairs
The House Affordable Medicines Caucus recently launched by Reps. Peter Welch (D-VT) and Keith Rothfus (R-PA) already has plenty of ideas to reform our nation's drug policies and produce cost savings for both the federal government and beneficiaries. The latest edition of Health Affairs (subscription required), though, adds a couple more ideas to encourage more efficient use of prescription drugs.
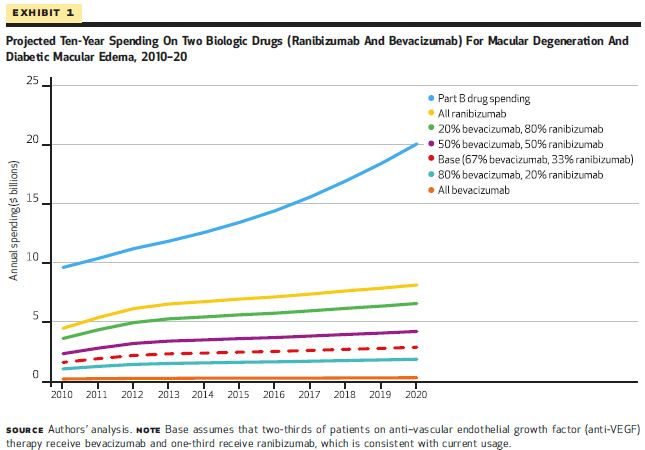
The first article from authors David Hutton, Paula Anne Newman-Casey, Mrinalini Tavag, David Zacks, and Joshua Stein takes a closer look at two popular drugs, Avastin and Lucentis, used to treat two of the leading causes of blindness. Although the drugs have been shown to have similar effectiveness in government trials and so far seem to have only minor differences in the prevalence of side effects, Lucentis costs 40 times more per dose than Avastin. And these two drugs have been very popular, accounting for $2 billion in Medicare outlays in 2010, or one-sixth of all Part B drug spending, and $500 million in beneficiary spending. In terms of use, Avastin already accounts for two-thirds while Lucentis accounts for one-third.
In their study, the authors estimate that if all Medicare patients were instead prescribed Avastin, taxpayers would save $18 billion and patients $5 billion over ten years, drastically curtailing the share of Part B drug spending consumed by these two drugs, from one-sixth to just 2 percent. If non-Medicare patients were to switch as well, the overall savings would increase by another $6 billion to $29 billion.
The question, then, is how to encourage greater use of Avastin in place of Lucentis. The path of least intervention likely flows through changing the perverse way Medicare reimburses physicians for administering drugs. Currently, physicians are reimbursed for the average sales price (ASP) of the drug plus an add-on intended to compensate for administrative costs equal to 6 percent of the drug's ASP. Tying a physician's reimbursement to the cost of a drug inevitably incentivizes him or her to use the most expensive drug available, regardless of whether a cheaper, therapeutically equivalent alternative is available. And given that 90 percent of Medicare beneficiaries have supplemental insurance that often covers most to all of their cost-sharing responsibility, very few beneficiaries will even pay the extra money the physician's decision would normally entail. Converting the percentage add-on to a flat payment regardless of which drug is administered would do a lot to increase the use of Avastin (and other less costly Part B drugs), as was recommended in the President's budget, by the National Coalition on Health Care, and by the Bipartisan Policy Center.
Or to provide an even stronger incentive, in the case of therapeutically equivalent drugs, Medicare could reimburse only to the ASP plus six percent of the least costly option. Doing this would achieve the full savings that the authors identify but requires Medicare to decide when drugs are perfectly substitutable and specify any exemptions to that dictate.
The chart below shows how drug spending swings depending on which drug is used (ranibizumab is Lucentis, bevacizumab is Avastin).
The second article from Yuting Zhang, Chao Zhou, and Seo Hyon Baik examines the automatic assignment of prescription drug plans to Medicare Part D beneficiaries who receive the Low-Income Subsidy (LIS) and do not voluntarily elect a plan. The LIS assists with premiums and cost-sharing for low-income beneficiaries in Part D. New LIS-eligible enrollees who do not indicate a preferred drug plan and current enrollees whose plan premiums exceed a certain amount are randomly assigned plans. This study attempts to measure the savings for beneficiaries and the government if they were assigned to a plan in their region that would best meet their needs.
They take a random sample of LIS enrollees who were randomly assigned plans in 2009 and compare actual prescription drug spending to the spending that would have occurred if they had been assigned to the plan that would have minimized their costs based on 2008 drug consumption. The authors note some limitations to their study, most notably that they assume no change in drug consumption patterns.
When enrollees are assigned to the optimal plan, the resulting savings to the government amount to $710 per person on average, which translates to $5 billion of spending in 2009. As noted above, the real world savings would be smaller because beneficiaries would change their consumption patterns to some degree based on the benefits of their new plan. In addition, the study looks only at one year, so it excludes any effect from insurance companies adjusting prices or or plan offerings based on policy changes that lead to a different mix of beneficiaries for a given plan. Regardless, policymakers should closely examine the issue of random versus intelligent plan assignment to determine effects on the budget and impacts on the LIS population.
Clearly, opportunities exist to assess Part D and Part B drug policy structure for potential savings, which should be balanced against incentives to innovate and other implications for the health system at large.

